Have you heard? Venture Capital firm General Catalyst bought a health system — specifically, Summa Health in Akron, Ohio. I’ve never been to Akron (though I do have family not too far away in Pittsburgh). GC is headquartered near me in Boston (Cambridge to be precise) with satellite locations in San Francisco, Palo Alto, London, and New York. Akron is a long way from those cities geographically and, I suspect, ideologically too. For some, a VC firm buying a health system is a long way from healthcare innovation. And yet, here we are.
Skepticism is standard operating procedure in healthcare. During our training, doctors are taught to think critically, question everything, and find hidden connections. Doing so can be the difference between delivering great care and missing a diagnosis. We are taught to view data through the lens of the scientific method. We’re supposed to be empiricists. But the competitive, high-stakes nature of medicine often warps our thinking and transforms empiricism into skepticism. Skepticism has its merits —protecting patients from harm — but is counterproductive when it becomes a self-protective defense mechanism. [It’s worth noting that healthcare skepticism isn’t limited to doctors. Patients are increasingly distrustful of a system they feel is failing them on multiple levels.]
Skepticism isn’t limited to the clinical practice of medicine, it’s prevalent in healthcare administration too. Physicians have become increasingly distrustful of healthcare machinery — most commonly the government (CMS), payors, and administrators. Many have become jaded toward a system that has slowly stripped away their autonomy and increasingly treated them like cogs in the machine, both expendable and interchangeable. Mounting frustrations and deepening skepticism have resulted in growing rates of burn out and drop out.
There are many fascinating angles to General Catalyst’s purchase of Summa Health and what it means for healthcare innovation. Corporate ownership of health systems isn’t new — private equity firms have been doing it for years. In my mind, VC and PE are opposite sides of the same coin — one side aims to grow a fledgling seed, the other aims to revive a dying plant. GC has deep roots in digital health. Buying a health system gives it a greenfield upon which to sow its many health tech seeds. Lowering the barrier to adoption, developing processes with a tech focus, and driving innovation through an integrated, ground up approach opens a world of possibilities. Skeptics — you can’t escape them in healthcare — would argue this move is little more than self-dealing and attempt to prop up a flagging portfolio. Does GC deserve the benefit of the doubt? Time will tell.
From the physician perspective, the most interesting aspect of the GC/Summa acquisition is what it means for the crumbling relationship between clinicians, patients, administrators, and other healthcare stakeholders. Frontline care delivery is at a troubling crossroads and, as often as this issue is highlighted on slide decks, true innovation seems lacking. The core of medicine will always be the relationship between those delivering care and those receiving it. Unfortunately, we are moving further away from this core competency toward a system that appears cynically focused on protectionism and silos. We seem locked in a never-ending battle over pieces of a pie that are somehow both growing (18% of GDP) and shrinking (another year of Medicare reimbursement cuts for docs) at the same time. The foundation of American healthcare is cracked and crumbling. Up to now, healthcare innovators seem largely content to build on top of this broken framework. It’s no surprise that so few efforts have had lasting impact. Buying a health system represents a unique opportunity to lay a new foundation. To me, that’s the most fascinating part of this whole thing.
There are various metrics by which GC’s purchase of Summa Health could be measured and deemed a success or failure. Can the firm take a non-profit (and not profitable health system) and make it a successful business? Can it drive widespread adoption of sustainable value-based care where others have failed? Can it maintain access to healthcare while improving outcomes and reducing costs? These are all important questions and valid KPIs by which to judge this effort. But, in my mind, success will only be achieved if GC and Summa can fix frontline healthcare by reversing burn out and restoring patients’ faith and trust in our healthcare system. Anything short of that is, to me, a failure.
Will it play out that way? Who knows? For what it’s worth, GC chose Marc Harrison to be CEO of what is currently being called “Health Assurance Transformation Corporation” or HATCo. I don’t know Mr. Harrison personally although he was kind enough to accept my LinkedIn connection request. (Thanks Marc!). His recent 6-year stint as President and CEO of Intermountain Health, itself viewed as a pillar of healthcare transformation, certainly speaks to his qualifications. Those that know him seem to feel that, if anyone can make this work, it’s Marc. That many have given unsolicited votes of confidence is encouraging.
On a personal note, my father was a career healthcare administrator who worked his way up from OR manager to hospital CEO. Growing up, I didn’t understand much about what his job entailed other than that his office was tucked away from clinical areas, and he had access to the doctor’s lounge where I could get free fountain drinks. His was an era where the balance of power still resided with physicians — a source of challenges and frustrations. Retired now, he’s more circumspect about his career — and willing to share his thoughts and experiences with me, his Orthopedic Surgeon son. When I went off to med school, his biggest piece of advice was “don’t be a jerk.” I’ve tried to honor that request. It’s for others to judge if I’ve been successful.
Based on my dad’s experiences, I’m sympathetic to the challenges of running hospitals and health systems. In today’s healthcare, the skepticism, cynicism, and divide between clinicians and administrators runs deep. This disconnect has downstream effects and undeniably impacts frontline care delivery contributing to burnout and declining trust in the medical establishment. Herein lies GC/Summa Health’s greatest opportunity (and perhaps its biggest challenge) — build a better foundation. From a doctor’s perspective, the keys to achieving this goal include giving clinicians a seat at the table, restoring autonomy and ownership, and resurrecting the doctor-patient relationship.
A Seat at the Table
When doctors whinge about the current state of healthcare, one of our biggest laments is that, somewhere along the way, we lost our seat at the table — literally and figuratively. A recent AHA survey found that almost one-third of non-profit hospital boards had zero physicians and two-thirds had zero nurses. STAT news reported further highlighted this issue, detailing disappointing findings regarding hospital boards at some of the most highly ranked non-profit academic medical centers. Less than 15% of board members at these institutions are healthcare workers — just 13.3% are physicians and 0.9% are nurses. Meanwhile, 44% of board members come from the financial sector. Based on these findings, clinicians quite literally lack a seat at the table.
While hospital boards aren’t the end all and be all of decision-making and governance, these findings hint at a bigger and more significant trend — the loss of meaningful input. Having demonstrable influence and a hand in shaping policies, procedures, direction, and culture is more important than a token leadership position. The rift between healthcare workers and administrators is real and represents a disconnect between the C-suite and the OR suite, outpatient clinic, inpatient floor, ER, etc. Frontline staff no longer feel heard and increasingly feel that their opinions don’t matter.
I have never been employed by a hospital or health system. The first 13 years of my career were spent in private practice, and the last two as part of a private equity-backed MSO. However, I've had my fair share of seats at the table including stints as Medical Director of Orthopedics, Joint Replacement Service Line Director, Department of Surgery Committee member, and a handful of other leadership roles with an administrative component. I currently participate in a Musculoskeletal Quality Collaborative for a 14-hospital health system and serve as Total Joint Director for an Ambulatory Surgical Center. Often in these roles, the literal seat doesn’t translate to a figurative seat. What do I mean by this cryptic and overwrought metaphor? Simply put, there is far too much talk (and So. Many. Meetings.) and not enough action. To be fair, enacting change and aligning incentives is difficult. The bigger the group, the harder it is. Doctors aren’t blameless here either. We could do a better job of listening and adopting a collaborative mindset while being less (gulp) skeptical. But I walked away from some of these positions because, after a while, you simply don’t feel heard. If none of your ideas are getting through and talk never translates to action, you quickly learn there are better ways to spend your time. (I once witnessed a hospital pay a consulting firm tens of thousands of dollars to make the OR more efficient. The consulting firm endorsed many of the same recommendations surgeons had been making for years. Ultimately, due to institutional inertia and lack of admin buy-in, few of the improvements were enacted. Despite considerable time and money spent, little changed).
In conclusion, clinicians should be given meaningful seats at the table. They should be present when important decisions are made and should be able to tangibly influence those decisions. The illusion of representation isn’t any better than no representation at all. Having deep clinician involvement at all levels is a sign of a confident and forward-thinking organization. Treating clinicians as mere figureheads maintains the clinician-admin divide — and the status quo.
Restoring Autonomy and Ownership
Loss of autonomy is one of the biggest drivers of clinician burnout and contributes to loss of ownership. We are in an unprecedented era in medicine where more physicians are employed than independent. Given current market conditions (declining reimbursement, rising practice costs), this trend is highly likely to continue. For many physicians, consolidation means relinquishing autonomy and ownership. It doesn’t have to be that way.
Autonomy means making independent decisions, acting in the best interest of patients, and emphasizing clinical decisions above business concerns. There is an epidemic of policies, procedures, and regulations that increase barriers to care and strip away clinical autonomy while rarely leading to demonstrable improvements in quality or outcomes. Some would argue that this is a symptom of the explosion of administrative layers. Others would point to the constant intrusion of non-clinical entities and middlemen onto the frontlines. Yet others would blame micromanagement and unrealistic expectations to do more with less. Although some of these issues are beyond the direct control of a health system, supporting physicians by fostering autonomy is possible. Advocating for physicians when it comes to dealing with payors, the government, EHR companies, and the broader healthcare industry would go a long way to restoring autonomy. Clinicians are desperate for an influential partner willing to go to bat with them. Again, a mature organization is one that fosters physician autonomy instead of fearing it.
Loss of autonomy fosters a sense of frustration and hopelessness — and eventually a loss of a sense of ownership. How can you feel invested in something when you’re treated like an interchangeable cog in the machine? If you surveyed healthcare workers, how many would say they feel a sense of pride or deep connection to their hospital or health system? We all want to feel valued and that the work we’re doing has meaning. Too often in healthcare, token gestures have taken the place of meaningful efforts to foster a sense of autonomy and ownership. I’m certain most doctors would trade a free breakfast or mindfulness session for fewer hoops to jump through and more initiatives to restore ownership.
One of the most important lessons I’ve learned as a physician is that quality and efficiency are driven by fostering a sense of autonomy and ownership. In the operating room, it starts at the top with me as the surgeon. It’s incumbent on me to be respectful, make sure everyone feels empowered, and lead by example. Whether it’s in the hospital, the ASC, or the clinic, patients can sense the difference between a well-functioning team and a dysfunctional one. The key to high quality, high value care is a team that thrives on ownership and autonomy.
A fantastic way to foster ownership is to give ownership. No, doctors still can’t own hospitals. But there are ways to provide clinicians with some skin in the game such as co-management agreements, gainsharing, and quality incentive programs. These initiatives work best when both sides’ interests are fairly represented. Though I’m no expert on the regulatory issues surrounding ownership structures, it seems plausible that GC could develop creative ways to give doctors, nurses, therapists, etc. an ownership stake in their health system, through an MSO structure or other management entity. Literal ownership is one of the most effective ways to drive figurative ownership.
Resurrect the Doctor-Patient Relationship
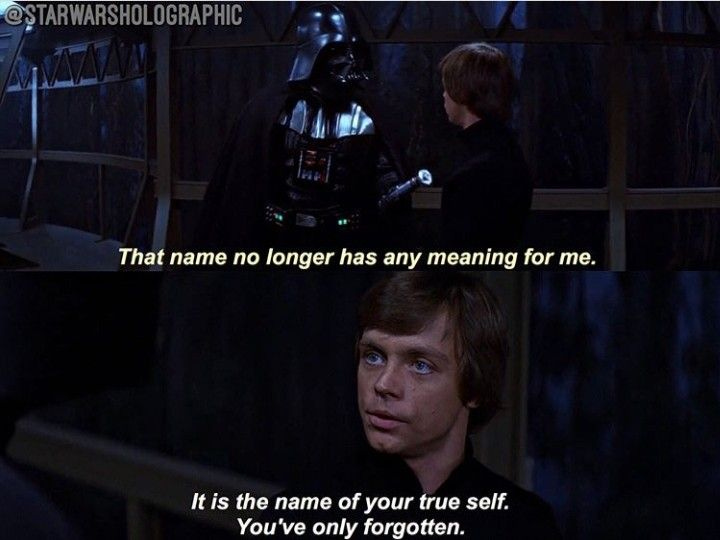
The core of healthcare has been and always will be the doctor-patient relationship (and more broadly, the relationship of the patient to the healthcare system writ large). Many feel that the term doctor-patient relationship no longer has any meaning.
Sadly, yes, we have forgotten. What does it mean to resurrect this relationship? Though it may seem unlikely, I believe many “innovations” that have yet failed to provide sustainable, meaningful impact in healthcare have a role to play here. Value-based care, properly implemented, can place emphasis back on doing what’s right for patients and incentivizing better care (not more care). The key, of course, is getting it right. No more race to the bottom. No more spurious metrics. No more upcoding or complexity hacking. Reward great care. Build systems from the ground up instead of trying to retrofit flawed processes onto a broken foundation. GC has a unique opportunity to take a fresh approach to VBC. A big part of that will be successfully aligning incentives with other stakeholders including doctors, payors, vendors — and patients too. In theory, VBC is very much about resurrecting the doctor-patient relationship. In practice, few have been able to hit on the right formula.
General Catalyst has a deep bench of health tech portcos (a category they call “health assurance”). Skeptics (them again) would argue that digital health has had minimal impact on healthcare, despite much hype and many dollars. Cynics would argue GC’s purchase of Summa Health is a thinly veiled attempt to prop up a flagging sector and minimize investment losses. The promise of health tech has always been to bring medicine into the 21st century by leveraging technology to improve access, outcomes, and quality. There are assorted reasons why these efforts have failed, many of which revolve around traditional system hurdles such as long sales cycles, institutional inertia, workflow disruption concerns, traditionalism, silos, and (yep) skepticism. All these barriers can be overcome if stakeholders pull in the same direction. Technology must be thoughtfully implemented rather than forced upon a system that isn’t ready for it. Digital health was always going to work best as a tool of an evolved system rather than a force for evolution. Here’s a chance to test that hypothesis.
Finally, in my mind, resurrecting the doctor-patient relationship is possible if we really want it. Doing so means changing our mindset around what healthcare delivery should be. Patient engagement and activation are critical to achieving superior outcomes. Technology can play a role here. Clinicians with a sense of ownership/autonomy and a seat at the table will feel empowered to deliver great care. If GC takes the path of first laying down a new foundation, then building upon it, we may see true healthcare disruption. If they are content to simply leverage existing mechanisms to drive profitability while self-dealing in poorly implemented health tech, this effort is a lot less interesting. VC’s owning a health system is bold and exciting until it isn’t. Doing more of the same isn’t innovative, no matter who’s pulling the strings. We’re at the unfortunate point in healthcare where many of the ideas expressed here would be considered radical. A VC firm buying a health system could be radical too — in a good way.








Ben: We all desire and hope for the creation of an ideal healthcare system model, one brimming with innovation and efficiency for both patients and physicians. However, as I mentioned in my latest piece on this deal, confining yourself to a tiny box by borrowing money, while also pledging to avoid cost cuts through layoffs, presents a risky proposition for all parties involved - patients, physicians, and investors alike. Time will tell… https://open.substack.com/pub/sergeiai/p/we-bought-a-hospital-we-couldnt-afford